RSV
Last updated Aug. 22, 2025.

RSV (respiratory syncytial virus) is a common respiratory virus that usually causes mild, cold-like symptoms. Most people recover in a week or two; however, RSV may lead to more severe outcomes and may require hospitalization, particularly among babies and older adults.
RSV can spread when:
- Someone with RSV coughs or sneezes.
- Virus droplets from a cough or sneeze get in your eyes, nose, or mouth.
- You have direct contact with the virus, like kissing the face of a child with RSV.
- You touch a surface that has the virus on it, like a doorknob, and then touch your face before washing your hands.
Some people can get immunized to protect themselves or their babies from serious RSV illness.
RSV vaccine for those who are pregnant

One way to protect your baby from getting very sick from RSV is to get vaccinated before you give birth.
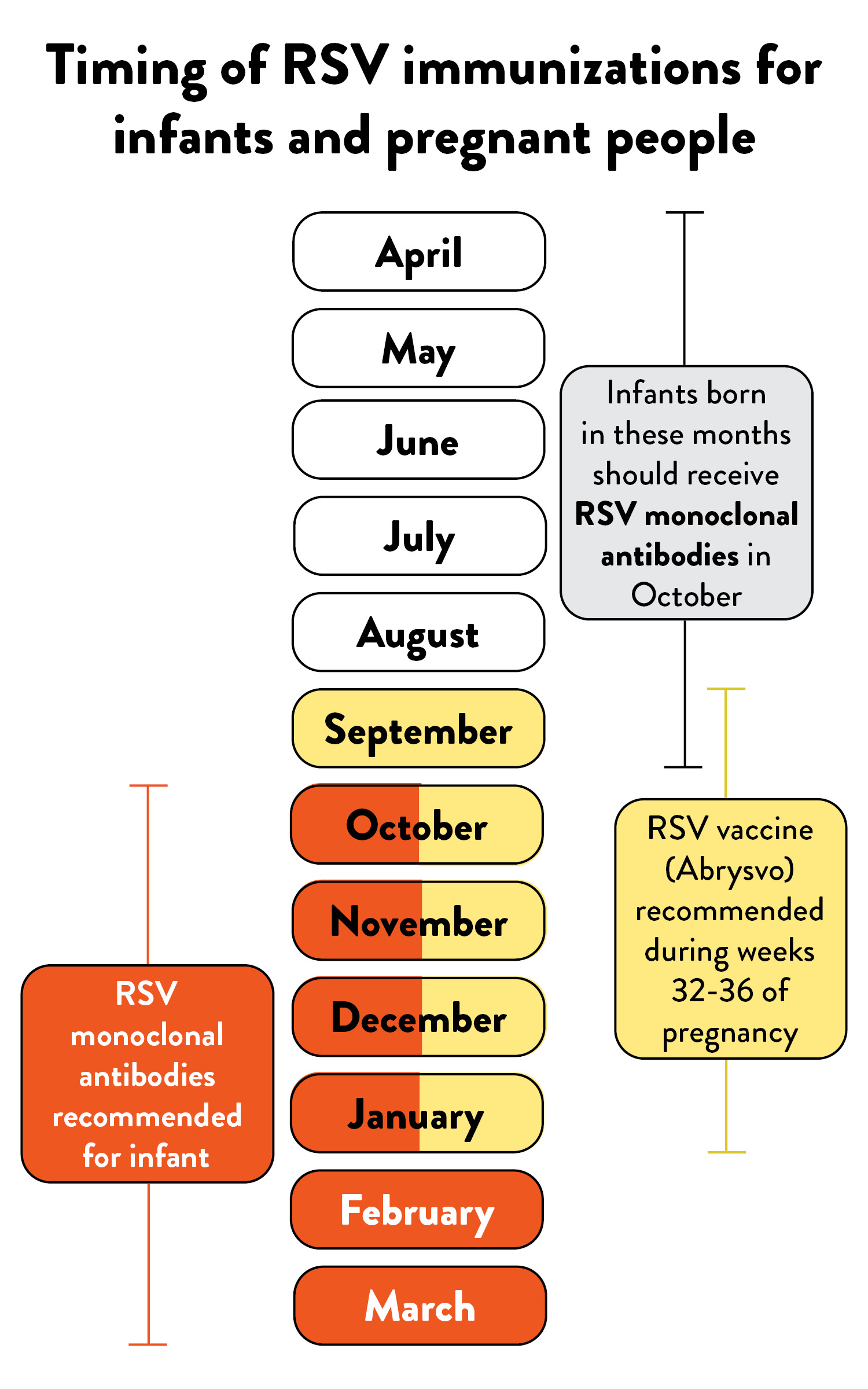
CDC recommends that those who are pregnant receive a single lifetime dose of RSV vaccine called Abrysvo during weeks 32 through 36 of pregnancy from September through January. This vaccination can help protect babies from serious RSV illness after they are born.
Those who are pregnant naturally give antibodies — germ-fighting proteins — to their babies during pregnancy. Because babies need time to develop their own immune systems, the antibodies they receive before they are born are crucial to protect them from diseases during the first few months of life and when they are too young to receive most vaccines.
When someone who is pregnant gets the maternal RSV vaccine, their body makes antibodies that protect against RSV. They then pass those antibodies on to their baby. These antibodies help protect the baby, significantly reducing their risk of being hospitalized in the early months of life. Babies who are born at least two weeks after a pregnant person gets vaccinated have a reduced risk of severe disease, particularly in the early months of life.
If you are pregnant, ask your prenatal care provider if you should receive an RSV vaccine during this pregnancy. If you do not have health insurance, or you have insurance that does not cover the full cost of vaccines, you may be eligible for a RSV vaccine at low or no cost from a public vaccine provider, or you may be eligible for a free RSV vaccine through Pfizer’s patient assistance program, Pfizer RxPathways.
RSV immunization for babies and some young children

Babies younger than 8 months can get a preventive monoclonal antibody during their first RSV season. These antibodies have been shown to greatly reduce the risk of both hospitalizations and health care visits for RSV in infants.
There are two monoclonal antibody formulations available for infants younger than 8 months: nirsevimab (BeyfortusTM) and clesrovimab (EnflonsiaTM).
RSV monoclonal antibodies are given as an injection, like a vaccine, from October through March. They provide infants and toddlers with lab-made antibodies to protect against RSV. This protection is critical during a baby’s first RSV season, when they’re most at risk for severe illness. Most infants do not need protection from both the maternal RSV vaccine given before birth and an RSV monoclonal antibody. Since only a single lifetime dose of RSV vaccine is currently recommended for pregnant people, infants born to people with a history of vaccination during a previous pregnancy should receive RSV monoclonal antibody after birth, ideally during the birth hospitalization.
Some older infants and toddlers at higher risk of severe illness should get a dose of RSV monoclonal antibody during their second RSV season, when they are between 8 and 19 months old. Nirsevimab (BeyfortusTM ) is the only RSV monoclonal antibody approved for use in this age group, which includes:
- Children who have chronic lung disease from being born prematurely
- Children who are severely immunocompromised
- Children with cystic fibrosis who have severe disease
- American Indian and Alaska Native children
Talk with your child’s health care provider about the RSV monoclonal antibody immunization.
If your child is on Medicaid, does not have health insurance or has insurance that does not cover the full cost of vaccines, they are eligible for an RSV immunization at low or no cost from a Vaccines for Children provider. The Vaccines for Children program provides immunizations at low or no cost for children who are uninsured, underinsured, on Medicaid or Medicaid-eligible, and/or Alaska Native/American Indian. Call ahead to confirm whether the provider has nirsevimab.
Comparison of immunizations to protect infants
| Pregnancy Vaccine (Pfizer’s Abrysvo) | RSV monoclonal antibody | |
|---|---|---|
| Who is it recommended for? | People who are 32 through 36 weeks pregnant | Babies born to those who did not get the Abrysvo vaccine while pregnant and also a small group of young children (ages 8-19 months) at increased risk of severe RSV. |
| How does it work? | Pregnant person passes protection (antibodies) to baby during pregnancy | Baby receives protection (antibodies) directly |
| When is it recommended? | September - January | October - March |
| Who does it protect from severe RSV? | Baby | Baby |
| How long does protection last? | Approximately 6 months after birth | At least 5 months after immunization |
| Who should not get it? | People with a history of severe allergic reaction to any component of the vaccine OR Those who have already received a dose during a previous pregnancy | Children with a serious allergic reaction to any component of an RSV monoclonal antibody OR Babies who are already protected |
RSV vaccine for older adults

CDC recommends that all adults aged 75 years and older and adults aged 50–74 years who are at higher risk for severe RSV disease should receive a single lifetime dose of RSV vaccine.
Three RSV vaccines are available for older adults: Arexvy™ (GSK), Abrysvo™ (Pfizer), and mResvia™ (Moderna).
Adults aged 50 and older can be at greater risk than younger adults for serious complications from RSV, in part because immune systems weaken with age. In addition, certain underlying medical conditions may increase the risk of getting very sick from RSV, such as chronic obstructive pulmonary disease (COPD), asthma, and congestive heart failure.
If you are 50 years or older, talk with your health care provider about RSV vaccination, and ask your health insurance provider if they cover it. If you do not have health insurance, or you have insurance that does not cover the full cost of vaccines, you may be eligible for an RSV vaccine at low or no cost from a public vaccine provider, or you may be eligible for a free RSV vaccine through Pfizer’s patient assistance program, Pfizer RxPathways.
Everyday RSV prevention
You can take everyday prevention measures to help reduce the transmission of RSV and other respiratory illnesses.
- Stay home when you're sick.
- Cover coughs and sneezes with a tissue or your shirt sleeve, not your hands.
- Wash your hands often with soap and water for at least 20 seconds, or use an alcohol-based hand sanitizer with at least 60% alcohol.
- Avoid touching your face with unwashed hands.
- Avoid close contact with others who are sick, such as kissing, shaking hands, and sharing cups and eating utensils.
- Clean frequently touched surfaces, such as doorknobs and mobile devices.
- Some people may choose to wear a mask for extra protection from respiratory viruses. Be respectful of everyone’s choices.