Measles
At a glance
- Reporting timeframe: Immediately (by phone within 4 hours of suspected diagnosis)
- Individual cases need follow-up? Yes
- Timeline for patient interview: 24 hours
- Responsibility for investigation: Local public health agency
- CDPHE Program: Vaccine-Preventable and Invasive Diseases
- Mode(s) of transmission: Airborne via respiratory droplets or direct contact with respiratory droplets.
- Incubation period: 7-21 days (average 7-14 days).
- Infectious period: Four days before to four days after rash onset.
- Treatment: Supportive care. No specific antiviral treatment is available, but vitamin A administration under the direction of a physician, may be appropriate. See more information under “Treatment.”
- Prophylaxis: Post-exposure vaccination (MMR) given within 72 hours (preferred form of PEP) or immune globulin (IG) given within six days. IG is limited to infants under six months or if MMR is contraindicated. IG may be recommended for high-risk contacts outside of the MMR PEP window.
- Case exclusion criteria: Exclude from work, school, or child care and should voluntarily self-isolate at home until four days after rash onset (day of rash onset is counted as day 0).
- Close contact exclusion criteria: Close contacts who do not meet immunity requirements should be excluded from work, school, or child care and quarantine at home until 21 days after last exposure. See “Contact investigation” below for more details.
Contents
What and how to report to the Colorado Department of Public Health and Environment (CDPHE) or local public health agency
- All people suspected of having measles, whether or not laboratory data are pending or available, should be reported immediately.
- Suspect cases require immediate attention and should be reported by telephone to CDPHE or local public health agencies, or followed up with a telephone call if reported by fax or through the Reportal or EpiTrax. See below for phone and fax numbers.
Important telephone and fax numbers
CDPHE Communicable Disease Branch
- Phone: 303-692-2700 or 800-866-2759
- Email: cdphe_vpd@state.co.us
- After hours: 303-370-9395
- Fax: 303-782-0338
Purpose of surveillance and reporting
- Identify cases for investigation.
- Identify sources and sites of transmission and any additional cases.
- Identify exposed people, assure timely administration of prophylactic vaccination, and prevent further spread of the disease.
- Promptly identify clusters and potential outbreaks of disease.
- Monitor trends in disease incidence.
- Monitor vaccine coverage of at-risk populations.
Etiologic agent
Measles virus is an RNA virus with one serotype, classified as a member of the genus Morbillivirus in the Paramyxoviridae family.
Clinical description
Measles (also known as rubeola) is characterized by a prodrome of fever (as high as 105°F) and malaise, cough, coryza (runny nose), and conjunctivitis, followed by a maculopapular rash (rash images available on CDC’s website). The rash typically starts on the head along the hairline then spreads to the trunk and lower extremities. The rash has been described as a “bucket of measles” due to the way the rash spreads like it was poured down from the head to the body. Koplik spots, which are tiny white lesions on the buccal mucosa, sometimes appear during the prodrome.
Individuals who have been vaccinated or have previously had measles can have a modified disease presentation, with less severe symptoms and/or absent or atypical rash. Rashes in previously vaccinated Colorado cases have been initially mistaken for acne or bug bites.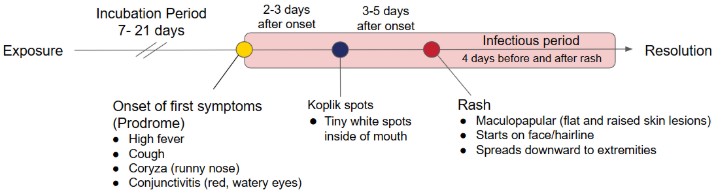
Approximately 30% of reported measles cases have one or more complications. Complications are more common among children younger than aged 5 years, and adults older than 20 years. Diarrhea, otitis media (ear infection), croup, and pneumonia commonly occur in young children. Acute encephalitis, which may result in permanent brain damage, occurs in approximately one out of every 1,000 cases. Death, predominantly due to respiratory and neurological complications, occurs in one to three out of every 1,000 cases reported in the United States.
Subacute sclerosing panencephalitis (SSPE) is a very rare but fatal long-term complication of measles. SSPE generally develops 7 to 10 years after a person has measles, even though the person seems to have fully recovered from the illness. The risk of developing SSPE is estimated to be 7–11 cases out of every 100,000 cases of measles. The risk of developing SSPE may be higher for a person who gets measles before the second year of life.
Treatment
No specific antiviral treatment is available.
Supportive care, including vitamin A administration under the direction of a physician, may be appropriate. Vitamin A does not prevent measles infection. Overuse of Vitamin A can lead to toxicity and cause damage to the liver, bones, central nervous system, and skin. Vitamin A dosing can be found on the CDC webpage, Clinical Overview of Measles.
Reservoirs
Humans are the only known host. An asymptomatic carrier state has not been documented.
Modes of transmission
Measles is transmitted primarily via large respiratory droplets or direct contact with infectious droplets. Airborne transmission via aerosolized droplet nuclei has been documented in closed areas (e.g., office examination room) for up to two hours after a person with measles occupied the area.
Incubation period
The incubation period is usually 8-14 days (range of 7-21 days). In rare circumstances, a person who is immunocompromised may have a longer incubation period.
Period of communicability or infectious period
Measles is highly communicable with greater than 90% secondary attack rates among susceptible people. Typically, a person is infectious for four days before to four days after rash onset.
Immunocompromised patients with measles may have prolonged shedding of the virus in their respiratory tract. They can be contagious beyond four days of rash and if hospitalized, should remain in airborne precautions for the duration of illness. See CDC Interim Infection Prevention and Control Recommendations for Measles in Healthcare Settings: Footnote 3 for list of severely immunocompromising conditions.
Epidemiology
Before the introduction of the measles vaccine in 1963, infection with measles virus was nearly universal during childhood, and more than 90% of people were immune by age 15 years. The highest incidence was among children aged 5-9 years, who generally accounted for more than 50% of reported cases. Following the licensure of the vaccine in 1963, the incidence of measles decreased by more than 98%. Fewer than 150 cases were reported each year from 1997–2004, and measles incidence decreased to a record low of 37 cases reported nationwide in 2004. However, the disease is still common throughout the world, including some countries in Europe, Asia, the Pacific, and Africa.
While measles is no longer endemic in the United States, cases and outbreaks continue to result from United States residents who travel abroad to places with measles and visitors to the United States. More recently, the United States has had several notable measles outbreaks. In 2024, Chicago experienced a measles outbreak of 57 cases associated with a migrant shelter. In 2025, a large measles outbreak with over 500 cases was identified in under-vaccinated communities in Texas and New Mexico. Outbreaks in the U.S. have historically been associated with insular communities with low vaccination rates. CDC maintains a summary of measles cases and outbreaks on its website.
Vaccination
Measles vaccine is incorporated with mumps and rubella vaccine or with mumps, rubella, and varicella as a combined vaccine (MMR or MMRV, respectively). The Advisory Committee on Immunization Practices (ACIP) recommends children routinely receive a first dose at 12 to 15 months of age and a second dose at school entry (ages 4 to 6 years). For children who were not vaccinated on schedule, providers should refer to the catch-up immunization schedule. Two doses of MMR are about 97% effective at preventing measles. One dose is about 93% effective. There is no single antigen (measles only) vaccine available in the United States.
Adults who received at least one dose of live measles-containing vaccine (which has been in use since 1968) on or after their first birthday should be protected against measles, but people in certain high-risk groups, such as health care professionals, students at colleges and universities, and those who plan to travel internationally, should have two doses or other evidence of measles immunity.
People who were vaccinated prior to 1968 with either inactivated (killed) measles vaccine or measles vaccine of unknown type should be revaccinated with at least one dose of live, attenuated measles vaccine (MMR). A killed measles vaccine, which was available from 1963-1967, was not as effective.
Most people born before 1957 do not need to be vaccinated because they likely developed immunity to measles during childhood when the disease was widespread. However, they may need MMR vaccine or other proof of immunity if they belong to certain high-risk groups like health care personnel.
Colorado law (6 CCR 1009-2) requires students attending child care, school, and college and university to be current on all school-required vaccines, or have an exemption in place.
- Child Care: One dose of MMR is required by 16 months of age.
- School age children: Beginning at kindergarten entry, two doses of MMR are required.
- College and university: Beginning at school entry, two doses of MMR or other evidence of immunity (i.e. birth before 1957) are required.
An acute illness characterized by the following a:
- Generalized maculopapular rash lasting three or more days; AND
- Temperature 101.0°F (38.3°C) or higher; AND
- Cough, coryza, or conjunctivitis.
Confirmed
An acute febrile rash illness (temperature does not need to reach ≥101°F/38.3°C and rash does not need to last ≥3 days) with:
- Isolation of measles virus from a clinical specimen; not explained by MMR vaccination during the previous 6-45 days; or
- Detection of measles-virus specific nucleic acid from a clinical specimen using polymerase chain reaction (PCR); not explained by MMR vaccination during the previous 6-45 days; or
- IgG seroconversion or a significant rise in measles immunoglobulin G antibody using an evaluated and validated method; not explained by MMR vaccination during the previous 6-45 days; or
- A positive serologic test for measles IgM antibody not explained by MMR vaccination during the previous 6-45 days and not otherwise ruled out by other confirmatory testing or more specific measles testing in a public health laboratory; or
- Direct epidemiologic linkage to a case confirmed by one of the methods above.
Probable
In the absence of a more likely diagnosis, a case that meets the clinical description, with non-contributory or no measles lab testing, and is not epidemiologically linked to a laboratory-confirmed case.
Note: CDC does not request or accept reports of suspect cases, so this category is not used for national reporting.
Epidemiologic classification: Confirmed cases should be classified as internationally imported cases or U.S.-acquired cases. A detailed travel history, including dates of travel and travel destinations, are needed to classify measles cases.
Collection of specimens for PCR and serologic testing is recommended for patients when clinical illness, vaccination history, and exposure history indicate a high suspicion for measles. Physicians should be instructed to obtain clinical samples from suspected cases at first contact.
To minimize false-positive laboratory results, case investigation and laboratory tests should be restricted to patients most likely to have measles. Important considerations are:
- Is the patient susceptible to measles?
- Does the patient have potential exposure to measles in the past three weeks?
- International travel
- Travel to an area with a measles outbreak
- Contact with a suspected or confirmed case of measles
- Does the patient have an illness clinically compatible with measles?
- Fever (greater than 101°F) and
- Generalized maculopapular rash and
- At least one of the "Cs" (cough, coryza, or conjunctivitis)
PCR, IgM, and IgG can all be positive in recently vaccinated people. If a person is highly suspected of having measles and they were recently vaccinated, a throat or nasopharyngeal (NP) swab should be collected for measles virus detection and genotyping at a public health lab.
Virus detection (PCR and culture)
- The preferred specimens for PCR testing are throat or nasopharyngeal swabs (ideally collected within three days of rash onset, but up to 10-14 days post-rash may be successful). PCR testing can also be done on urine and may improve sensitivity of testing, especially among vaccinated individuals. Clinical specimens for PCR should be collected at the same time as samples taken for serologic testing.
- Highly suspicious measles specimens should be sent to the Colorado State Public Health Laboratory for expedited PCR testing under the direction of a CDPHE Vaccine Preventable Disease (VPD) epidemiologist. This testing is performed on a fee-for-service basis. CDPHE does not have public health funding to cover measles testing.
- Visit CDPHE’s Measles (Rubeola), RT-qPCR webpage for additional information such as specimen collection, packaging specimen for transport, and testing costs.
- Low-suspicion measles specimens can be sent to commercial labs that offer PCR testing for measles or to the CDPHE Lab. Testing for low-suspicion measles samples will not be expedited or conducted after hours at the CDPHE Lab.
- Positive PCR in patients with an acute febrile rash illness is confirmatory unless explained by recent MMR vaccination (during the previous 6-45 days) or not otherwise ruled out by other confirmatory testing or more specific measles testing in a public health laboratory.
- Isolation of measles virus in culture is confirmatory (unless the patient was recently vaccinated), but measles culture is rarely done.
- A negative culture or negative PCR does not always rule out measles because both methods are affected by the timing of specimen collection and the quality and handling of the clinical specimens.
- Please visit How to test for measles at CDPHE for testing at the CDPHE lab.
Serology (IgM and IgG)
- Public health should recommend collection of a serum specimen to test for measles IgM at first report of a suspected measles patient.
- A measles IgG antibody test is most commonly used to determine immunity to measles while measles IgM tests for acute disease.
- Measles IgG and IgM tests should both be recommended.
- Cases with positive measles IgM results at a commercial lab may need to be retested at the Colorado State Public Health Laboratory if there is an indication the result may be a false-positive. The possibility of a false-positive IgM test is increased when: the IgM test used was not an enzyme immunoassay (EIA), the case did not meet the clinical criteria, the case is an isolated indigenous case (no epidemiologic link to another confirmed case and no international travel or travel to a place with an outbreak), the case was vaccinated within the last six months, or measles IgG was detected within seven days of rash onset.
State Laboratory testing services available:
- The Colorado State Public Health Laboratory charges a fee for measles testing. An invoice for the testing cost will be sent to the ordering medical provider or facility, who then typically refers to the patient or the patient’s insurance company. In very rare and high-risk situations where a suspect case is not able to cover the cost of testing, CDPHE may cover the cost of testing if approved by a CDPHE VPD epidemiologist. Recommending testing at the CDPHE lab is not an indication that the cost of testing will be covered by CDPHE.
- The Colorado State Public Health Laboratory can perform measles PCR testing on respiratory specimens or urine. Some commercial labs are able to perform measles PCR testing as well.
- Serologic testing for measles IgM antibodies can be done through the Colorado State Public Health Laboratory and commercial laboratories.
- Measles IgG antibody test is available at most commercial labs and some hospital labs. It is not available at the Colorado State Public Health Laboratory.
Local public health agencies have primary responsibility for investigating reports of suspected, probable, and confirmed cases in their jurisdiction. CDPHE VPD epidemiologists are available to help local public health agencies investigate cases, as needed.
Use “Questionnaire for people suspected of having measles” on the CDPHE measles webpage and the measles investigation form found on CDC’s website to help with collecting pertinent information. Information from the surveillance form should be entered into EpiTrax within three business days of the interview. During urgent responses, more timely data submission may be required. Paper forms do not need to be faxed to CDPHE.
- Determine whether the symptoms of an individual with suspected measles are compatible with measles.
- Measles is rare in Colorado, and clinical evidence is not sufficient to confirm a case. Laboratory diagnosis is crucial to confirm the few actual measles cases among the many patients with suspected measles.
- In communities where measles cases or outbreaks are occurring, suspicion for clinical diagnosis should increase.
- Gather clinical information through medical record review or by interviewing the case, the case’s guardian, and/or the case’s health care provider. Collect the following information:
- Demographics (including address, phone number, date of birth, gender, ethnicity, and race)
- Timing and sequence of symptoms:
- When did the fever start? How long did it last? What was the maximum temperature?
- When did the rash start? Where on the body did it start? What did it look like? How did it progress? How long did it last?
- Were there other respiratory symptoms (cough, coryza, and conjunctivitis)?
- Are there other possible diagnoses?
- What lab tests are available? What is pending?
- Has this person recently taken antibiotics or other medications?
- Does the patient have contacts with similar symptoms?
- Determine if the case is susceptible to measles.
- Obtain documentation of immunization history, including MMR/MMRV vaccination dates from the medical provider, the case or case’s guardian (if conducting a patient interview), and by checking the Colorado Immunization Information System (CIIS).
- People born in the United States prior to 1957 probably had measles disease during childhood and are likely immune.
- To note, if the patient was recently vaccinated, they may have a positive PCR or IgM test result despite not having the actual disease.
- Determine if the case was exposed to measles.
- Ask about recent travel within Colorado to places with known measles exposures, travel outside of Colorado, and travel outside of the United States. Document specific places and dates of travel.
- Detail the patient’s activities 7-21 days prior to rash onset, including travel or visitors from other countries or other states.
- Ask the case if they had contact with other people who are ill.
If the suspected case DOES NOT have clinically compatible symptoms, a likely exposure to measles, or susceptibility to measles, consult with CDPHE before proceeding with the investigation. Testing may still be indicated but contact investigation can wait for laboratory results. |
- If a suspect case is determined to have high likelihood for measles (including symptoms clinically compatible with measles, a likely exposure to measles, and is susceptible to measles):
- Obtain appropriate diagnostic specimens (respiratory and blood specimens) and immediately arrange testing with a CDPHE VPD epidemiologist. See how to test for measles at CDPHE.
- Establish a timeline of the patient’s activities and contacts while they were infectious (four days prior and four days after rash onset, with the day of rash onset counted as day 0) including but not limited to:
- Household members (significant others, children, dependents, etc.).
- Visits to public areas like stores, restaurants, and health care facilities.
- Attendance at school or work.
- Social/religious/family events or gatherings.
- Travel history (domestic or international).
- Modes of transportation (rideshare, public transportation, personal vehicle).
- House visitors/guests (cleaners, dog walkers, food/grocery delivery services, etc.).
- Hospital visitors.
- Exclusion:
- People suspected or confirmed of having measles should be excluded from work, school, or child care and should voluntarily self-isolate at home until for days after rash onset (day of rash onset is counted as day 0).
- In health care facilities, patients suspected of having measles should be placed in a negative pressure room. If a negative pressure room is unavailable, place the patient in a room alone with the door closed. CDC has infection prevention and control recommendations for measles in healthcare settings on their website.
- Ensure only people who are immune to measles are allowed to come in contact with the case until at least for days after rash onset.
If multiple attempts to obtain case information are unsuccessful (e.g., the case, case’s guardian, or health care provider does not return your calls, or the person refuses to divulge information), contact a CDPHE epidemiologist to discuss other options.
Once a confirmed or highly suspect case is identified, initiate an investigation to determine where exposures may have occurred and who were in those spaces. The main purpose of identifying contacts is to determine which contacts are susceptible to measles and provide appropriate disease control recommendations.
- Identify places where exposures occurred.
- Using the infectious period established during the case investigation, identify settings and times where exposures may have occurred.
- Measles investigations are time-sensitive and often involve a large number of contacts, so it is recommended to focus first on people at highest risk of disease transmission.
- Prioritize initial contact investigation and disease control efforts on people in settings with prolonged, close proximity to the case such as households, child care facilities, schools, health care settings, and congregate settings, such as churches and other institutions (colleges, prisons, etc.).
- Work with the setting (i.e., the health care facility, school, child care center, etc.) to obtain a list of people who were in the same location as the case or in those areas up to two hours after the case was present and could have been exposed to measles.
- Categorize exposure settings by risk level
Exposure locations should be evaluated by public health and assigned a risk category based on proximity, duration of exposure, vaccination status of people in the setting, and presence of people at risk for severe measles disease.
High-risk exposures
Places where people have close, prolonged contact to others, places where there is low vaccination coverage, or places with people at risk for severe measles disease such as:
- Households
- School classrooms, child care centers, and extracurricular activities such as sports
- Health care settings such as outpatient clinics, urgent care centers, and inpatient facilities without advanced air ventilation
- Congregate living or shelters
- Settings where people gather who are immunocompromised or are not eligible to receive MMR vaccinations
- Places of work, such as office buildings, depending on the size and airflow in those spaces
Moderate-risk exposures
Places where close contact or interactions could have occurred, generally indoors or an enclosed setting with short to moderate duration of exposure, such as:
- Emergency department waiting rooms and other medical facility spaces with a higher level of air exchanges per minute
- Gatherings/meetings such as religious services, weddings, and fitness classes
- Airplanes, ride-share, trains, and buses
- Larger workplaces
Low-risk exposures
Places visited by members of the general population who may have had passing or indirect contact with the case, such as:
- Grocery stores, shopping malls, fast food restaurants, airports, or gyms
- Parts of a building that might share airspace with someone who had measles but where a measles case was not specifically present
- Assess measles immunity of contacts by exposure risk
To ensure consistent and accurate public health guidelines, assessment of immunity should be done by public health and not by a person’s employer, school, or health care provider. (One exception is that health care facilities can assess presumptive immunity of their own exposed staff members, but this should be done with oversight from public health and with public health providing clear guidelines to the facility on who should be considered presumptively immune.)
- High-risk exposures
- Should be assessed by direct, individual public health contact, preferably by phone.
- Moderate-risk exposures
- Recommend to be assessed by direct public health contact. However, if individual assessment exceeds a public health agency’s capacity, these contacts could be guided to their health care providers for assessment of immunity status and the need for PEP.
- Low-risk exposures
- Individual assessment of presumptive immunity should not be prioritized and in some settings (such as restaurants, stadiums, and large retail stores), might not be possible. In these situations, general recommendations around PEP are provided through various notifications (see “Notifications” section below), and those contacts are guided to their health care providers or the health department for assessment of immunity status and the need for PEP.
People meet presumptive evidence of immunity if they meet one of the following criteria (note: see criteria below for contacts who are health care personnel or people who are severely immunocompromised):
- Age-appropriate measles-containing vaccination*:
- One or more documented doses of a measles-containing vaccine administered on or after the first birthday for preschool-age children and adults not at high risk
- Two documented doses of measles-containing vaccine for school-age children, adolescents, and adults at high risk, including college students, health care personnel, and international travelers
- People with one MMR who are in an age group or risk group recommended to receive two doses should get another MMR as soon as possible after exposure.
- Laboratory evidence of immunity (i.e., a positive measles IgG titer)
- For people who are likely immune to measles but lack necessary documentation (e.g., an adult household contact who cannot find their vaccination record, or someone born after 1957 who recalls having disease as a child), IgG positive counts as evidence of immunity.
- Detection of IgG in an asymptomatic contact can be an indication of pre-existing immunity to measles through either prior vaccination or prior measles infection.
- Specimens for measles IgG testing in close contacts should be collected as soon as possible after exposure, as IgG will rise if symptoms develop.
- High-risk contacts with uncertain immunity should remain quarantined until results are available.
- IgG testing is not available at the CDPHE Lab. People who need IgG testing to determine their immunity should contact their health care provider for specimen collection and testing at a commercial laboratory.
- Laboratory confirmation of a measles infection prior to recent exposure
- Birth before 1957
For contacts without high-risk exposures, the following criteria could be used additionally in consult with CDPHE if presumptive evidence of measles immunity is not available of individuals during a large public health response to prioritize identifying and providing PEP to those most likely to be susceptible:
- Compelling history of measles vaccination, such as:
- Self-reported dates of vaccination
- Served in the U.S. armed forces
- Entered the United States in 1996 or later with an immigrant visa or a green card
- Compelling history of disease, such as coming from a country where measles is or was endemic
Considerations for special populations who are more likely to transmit disease to vulnerable people or at risk for severe disease if they develop measles
- People who are pregnant
- Infants < 12 months
- Health care personnel are more likely to transmit disease to vulnerable people if they become ill and must be evaluated carefully. See “Managing special situations: health care facilities” below.
- People who are severely immunocompromised are at risk for severe disease or longer infectious period if they develop measles and could be susceptible to measles despite previous vaccination. The degree of altered immunocompetence in a patient should be determined in consultation with their health care provider. CDPHE Medical Epidemiologists are available to coordinate these discussions and help determine if contacts are severely immunocompromised and meet criteria for IG. See RedBook for most current recommendations. Severely immunocompromised people include:
- People with severe primary immunodeficiency (RedBook: Measles, Table 3.33 , footnote B);
- People who have received a hematopoietic cell transplant until at least 12 months after finishing all immunosuppressive treatment, or longer in patients who have developed graft-versus-host disease;
- People on treatment for acute lymphoblastic leukemia (ALL) within and until at least 6 months after completion of immunosuppressive chemotherapy;
- People with HIV with severe immunosuppression, which for children ≤5 years is defined as CD4+ T-lymphocyte percentage <15% and for children >5 years and adolescents is defined as a CD4+ T-lymphocyte percentage <15% or a CD4+ T-lymphocyte count <200 lymphocytes/mm3, and those who have not received MMR vaccine since receiving effective antiretroviral therapy.). See RedBook for most current dosage information.
4. Determine disease control guidance for contacts
- Provide contacts with disease control recommendations based on exposure and susceptibility to measles as outlined in “Disease control recommendations for contacts” section below.
5. Public communication about exposure locations
- Work with the DCPHR Communications team to ensure locations where public exposures may have occurred are included in Health Alert Network (HAN) messages, press releases, and on the CDPHE website.
- Information should include the location name, address, and specific times when people could have been exposed.
- CDPHE should make sure any places of business or facilities that are included in these communications are notified that their business or facility will be mentioned in public messaging prior to the messaging going out. This is typically done by the public information officer of the county where the business or facility is located.
ALL measles contacts:
All measles contacts, regardless of exposure risk, should be instructed to watch for measles symptoms for 21 days after last exposure and contact public health if they think they are developing measles. They should also be told that if they need medical attention, they need to contact a health care facility before entering and tell them about their exposure so arrangements can be made to minimize additional exposures.
People without presumptive evidence of immunity:
Disease control recommendations for people identified as susceptible to measles are based on their exposure, risk of developing severe disease, and risk of spreading to others.
Disease control recommendations by exposure risk
High-risk exposures
Moderate-risk exposures
Low-risk exposures
- For healthy infants aged 6-11 months, MMR vaccine is preferred to IG if the exposure to measles occurred within 72 hours. MMR doses for children < 12 months are for immediate protection against a measles exposure and do not count towards vaccine recommendations. MMR is contraindicated for infants < 6 months.
- IG should be administered within six days of exposure and can extend the incubation period for measles. Monitor contacts who received IG for 28 days after last exposure to the case. IG PEP should be prioritized for contacts exposed in settings with intense, prolonged, and close contact (e.g., household, daycare, classroom) and is often not recommended in low-risk settings, but it can be considered for those at high risk of severe disease.
- Exclude from high-risk settings (e.g., health care, child care, schools) from Day 7 (Day 5 for health care personnel) after first exposure through Day 21 (or day 28 if IG PEP was received) after last exposure.
- People who receive IG PEP should be excluded from health care settings from Day 7 after first exposure through day 28 after last exposure. In other settings such as child care, schools, or workplaces, factors such as the intensity and duration of their exposure, vaccination status of people in the setting, and presence of populations at risk for severe measles disease should be taken into consideration when weighing the risks and benefits of excluding those receiving IG PEP.
- If it can be done rapidly, recommend that people who are pregnant be tested for measles IgG prior to receiving IGIV if there is a possibility they received a vaccine or had disease. Administer IGIV if the patient is IgG negative, or has unknown status and testing cannot be completed by Day 6 after exposure.
- There is no public health recommendation for IGIM in susceptible people > 30 kg (66 lbs). If within 72 hours of exposure, MMR is preferred for people > 6 months old without a contraindication to MMR. An intravenous version of IG (IVIG) is available for people who qualify for IG and cannot get MMR or IMIG, such as those who are pregnant or immunocompromised. See “Immune globulin (IG)” section below for more information.
- If implemented, quarantine should last from Day 7 after first exposure through Day 21 (or day 28 if IG PEP was received) after last exposure. Active monitoring can be considered as an alternative to quarantine for people without high-risk exposures. Quarantine is not recommended for people with low-risk exposures.
Additional guidance for disease control recommendations for contacts
- Post-exposure prophylaxis (PEP)
Measles vaccination (MMR)
- MMR vaccine is recommended for people exposed to measles who do not have evidence of measles immunity and for whom vaccination is not contraindicated.
- Administration of MMR vaccine to susceptible contacts of a measles case may abort infection or modify the disease if given within 72 hours of the first exposure.
- If unable to receive MMR PEP within 72 hours after the initial exposure, non-immune contacts should still be recommended to receive an MMR vaccination to provide protection from future exposures, especially if there is ongoing transmission in a particular setting such as a household, child care, school, or work setting.
- MMR vaccine should not be given within six months to people who received intramuscular immune globulin (IMIG) or within eight months to people who received intravenous immune globulin (IVIG).
- In some studies, MMR PEP effectiveness is low (even though protection against future exposures is high) and likely depends upon the nature of the exposure, among other things. Exposed people who received appropriate MMR PEP may still be excluded from high-risk settings, educated to watch for measles symptoms, and call public health if they develop symptoms of measles.
- While the public health response to sporadic measles cases should focus on those who are completely unvaccinated and more likely to be susceptible, in certain settings and if resources are available, it may be appropriate for people with one dose of MMR to get a second dose as post-exposure prophylaxis.
Immune globulin (IG)
- IG can be given intramuscularly (IMIG) or intravenously (IVIG) within six days of exposure to prevent or modify infection.
- For most contacts, post-exposure MMR vaccination is preferable to IG.
- Dosage for IMIG is 0.5mL/kg (max 15 mL).
- Persons weighing >30 kg/66 lbs are unlikely to receive an adequate amount of measles antibody from IMIG so IVIG should be considered.
- IMIG is recommended for exposed infants and children weighing <30kg/66lbs who do not have evidence of measles immunity or cannot get MMR.
- IVIG is recommended for exposed adults who do not have evidence of measles immunity and cannot get MMR (such as pregnant people) and those who are severely immunocompromised. It is typically maintained by hospitals and administered in health care facilities.
- Neither IMIG or IVIG are indicated for household or other close contacts who received one dose of vaccine at 6 months or older unless they are immunocompromised.
- People who received IMIG or IVIG should not receive MMR vaccine within six months of receiving IMIG or within eight months of receiving IVIG.
- IMIG and IVIG can extend the incubation period for measles; monitor contacts who received IG for 28 days after last exposure to the case.
- CDPHE maintains stock of IMIG in 2 ml and 10 mL single dose vials. IG is costly and has a relatively short shelf life. CDPHE-supplied IMIG may only be used for post-exposure prophylaxis.
- CDPHE maintains IMIG at two locations (one CDPHE location, one LPHA location). CDPHE is using a shared spreadsheet to track IG across the state; all LPHAs who receive IG for a response are expected to use this spreadsheet. To request IG please call the Communicable Disease Branch at 303-692-2700 (after hours 303-370-9395) or email cdphe_vpd@state.co.us. IG available through CDPHE is a state-purchased asset. In order for CDPHE to release IG, LPHAs must provide information about the planned use.
- Exclusion from high-risk settings
- Contacts of measles cases without presumptive evidence of immunity may be excluded from high risk settings but not limited to: health care settings, school, or child care. Exclusion may be used independently of quarantine.
- For low to moderate exposures, public health may recommend individuals without appropriate evidence of immunity or only have one documented dose of MMR to avoid high-risk settings or large gatherings.
- Symptom monitoring
- Active or passive symptom monitoring may be recommended for people exposed to measles who are at risk for developing and spreading disease.
- Active symptom monitoring:
- Public health should establish a communication plan with the contact that consists of an open line of communication to allow for daily or routine check-ins during the incubation period to ask about symptoms consistent with measles. This communication could include a combination of email, text message, electronic survey, or phone calls.
- Passive symptom monitoring:
- Public health educates the contact on signs and symptoms of measles and provides a phone number for the contact to use if he/she develops symptoms.
- If there is concern about the contact not reporting symptoms, active symptom monitoring may be recommended.
- If contacts develop symptoms during monitoring, instruct them to call their doctor’s office before seeking care and to wear a mask around people, especially if they will be going to a health care facility.
- Quarantine
- Quarantine is a process in which public health requires a person to stay at home for a period of time (typically from 7-21 days after) to prevent the spread of measles.
- It is not recommended to quarantine people with one MMR. They could be excluded from high-risk settings in specific situations such as if they were a high risk contact or during an outbreak.
- Quarantine can be a verbal agreement or a letter that outlines what should be done, but if there are concerns for compliance, a public health order should be issued.
- Consult with CDPHE VPD epidemiologists before placing a person in quarantine. Imposing quarantine measures is both difficult and disruptive, but may be necessary for disease control.
- A quarantine letter template is available upon request. Contact the VPD unit directly for a copy.
- The quarantine template is not intended as, nor should it be construed as, legal advice. Rather, it is meant to assist those preparing to issue an order of quarantine to think about the types of issues that one might address in such an order. Seek professional legal guidance prior to finalizing any public health order.
- CDPHE and LPHAs both have authority to issue quarantine orders.
- Consider arranging resources for quarantined people to help with compliance. This could include food delivery, job assistance, etc. Ensure only people who are immune to measles come in contact with the person in quarantine. CDPHE does not have resources to support individuals during quarantine.
- People under quarantine should be regularly contacted by public health to monitor for development of measles symptoms and ensure compliance.
- Isolation
- Isolation is the separation of sick people from well people.
- If someone develops symptoms consistent with measles, they should remain isolated at home or in a health care facility until they are no longer contagious.
- Notifications
- Different forms of notification can be used in the event of a measles case or outbreak, depending on the situation and urgency. Consult with CDPHE to determine the most appropriate way to notify contacts of their exposure.
- For low-risk exposures without individual contact tracing, media reports are used to notify people of their possible exposures. Those contacts will be guided to their health care providers or the health department for assessment of immunity status and the need for PEP.
- In some situations, hospitals or health care facilities will distribute a notification letter and guidance to patients, visitors and staff who were exposed to measles in their facility. It can be helpful to have this information come from a health care provider, but guidance related to disease control for measles (such as recommendations for post-exposure prophylaxis or quarantine) should be reviewed and approved by public health.
- A notification letter or emails can be used to broadly notify school or child care classmates about measles in the community, provide vaccine recommendations, and remind parents/guardians of exclusion policies for students with a vaccine exemption. This should be done in consultation with public health and with public health reviewing and approving guidance related to measles disease control.
- In response to some exposures, CDPHE can send text messages containing exposure information and a link to an online survey.
- The text/online survey approach can be used for large-scale exposures (for example, a church service) or for smaller scale, low-risk contacts, such as employees at a fast food establishment a case briefly visited.
- The text/online survey approach can be used to notify and gather information (presence at exposure location, immunity status, etc.) from contacts to prioritize further public health contact and action.
- A HAN Advisory or Alert about measles can be sent to health care providers and hospitals so they are prepared to identify and test measles cases. Sending a measles HAN should be discussed with CDPHE staff who can assist you in developing and distributing the notice either locally, regionally, or statewide.
- Social media posts and press releases are often helpful to alert the general public and provide vaccination recommendations for people who may have been exposed in places where it’s difficult to identify specific people, such as grocery stores and malls. Social media posts and press releases are typically coordinated between communication professionals at CDPHE, at the affected local public health agency, and at any other affected facilities.
- CDPHE can post a notification on CDC’s Epi-X forum to notify other states of potential exposures in their states or to request additional information on other cases.
- Hot Topics can be used to notify the health care community about the current situation.
- CDPHE will work with CDC to conduct contact notifications if a case was infectious while traveling on an airplane, train, or other similar conveyance.
Outbreaks
- A measles outbreak is defined as three or more related cases.
- The primary strategy for control of measles outbreaks is achieving a high level of immunity (i.e., two doses of measles vaccine) in the population affected by the outbreak.
- During a widespread measles outbreak:
- Guidance may be changed to recommend MMR vaccine to infants as young as 6 months old. This decision must be made with input from multiple partners, including the LPHA where the outbreak is occurring, the CDPHE Immunization Branch, the Medical Epidemiology Unit, and Communicable Disease Branch leadership and include planning for messaging and ensuring access to meet increased demand. Children immunized before their first birthday should still be immunized with MMR/MMRV vaccine at 12-15 months (at least four weeks after the initial measles immunization) and again at 4-6 years, before kindergarten entry. Some studies have demonstrated that immunization prior to 12 months might result in blunted measles antibody responses to routine MMR vaccines, which might be age-dependent.
- People who cannot readily document measles immunity should be vaccinated or excluded from the affected setting (school, hospital, child care). In an outbreak setting, only doses of vaccine with written documentation of the date of receipt should be accepted as valid.
- There may be additional recommendations for people with one valid dose of MMR vaccine to receive a second dose of MMR as long as it’s been 28 days after their first dose.
- Public health might also recommend people with one dose of MMR get a second dose as post-exposure prophylaxis.
- Verbal reports of vaccination without written documentation should not be accepted. People who have been exempted from measles vaccination for medical or nonmedical reasons should be excluded from affected institutions until 21 days after last exposure to a measles case and as long cases continue to occur in the facility.
- Under special circumstances, such as during outbreaks in schools attended by large numbers of people who are not vaccinated, restricting social events such as school dances, athletic events, and conferences might be warranted.
- A diagnosis of measles and measles testing should be highly considered in people with measles-compatible symptoms (rash and fever) in the outbreak-affected area.
- Intensify surveillance by providing measles information to hospitals, emergency rooms, urgent care clinics, physicians, schools, and child care providers.
- A diagnosis of measles and measles testing should be highly considered in people with measles-compatible symptoms (rash and fever) in the outbreak-affected area.
- Intensify surveillance by providing measles information to hospitals, emergency rooms, urgent care clinics, physicians, schools, and child care providers.
Health care facilities
People who work in health care settings are at increased risk of exposure to measles and at increased risk of transmission to people at high risk of severe measles. Health-care personnel (HCP) include all paid and unpaid persons working in health-care settings who have the potential for exposure to patients and/or to infectious materials, including body substances, contaminated medical supplies and equipment, contaminated environmental surfaces, or contaminated air. For this reason, health care personnel have different criteria for presumptive evidence of immunity.
Health care setting disease control recommendations
- Establish a point of contact at the health care facility (preferably the infection preventionist) who will gather information needed for investigation and disease control, such as lists of exposed health care personnel and patients and their immunity statuses.
- Create a timeline of the case’s movement within a health care facility. Determine what time the patient was in the waiting room, what time they were moved to an exam room, moved to a negative pressure room, or moved to other areas of the health care facility (such as the cafeteria, lab, x-ray, etc.). This information is used to determine who was exposed (staff and patients).
- As measles virus can spread through HVAC systems, it may be helpful to request a map of the facility and HVAC information to determine patient areas where the virus could have traveled.
- Request a list of patients with the following information: name, date of birth, address, staff/patient, phone number, location(s) of exposure, time(s) and date(s) of exposure.
- Notify exposed patients and visitors
- Patients who were in close proximity to the case (emergency department, waiting room, etc.) typically should be contacted by phone, especially if it is within the window to receive PEP (72 hours for vaccine, or 6 days for IG for individuals where IG PEP is recommended).
- For patients with minimal exposure (such as sharing a hospital floor, but on a different wing), a letter is usually adequate.
Patient disease control recommendations
- Managing hospitalized measles patient
- Patients who are diagnosed with measles while hospitalized should be isolated using airborne and contact precautions for four days after rash onset (with date of rash onset counted as day 0). Immunocompromised patients should be isolated for the duration of their illness because they may shed measles virus for extended periods.
- Hospitalized measles cases should be attended to and visited by only people who are immune to measles.
- Regardless of immunity status, all staff entering the room should use respiratory protection (i.e., a respirator) that is at least as protective as a fit-tested, NIOSH-certified disposable N95 filtering facepiece respirator.
- If possible, do not send the patient to other parts of the hospital for examination or testing procedures. When transport is necessary, the patient should wear a face mask, if tolerated. Use a transport route with minimal contact to other people. Notify health care providers in the receiving area.
- Use standard cleaning and disinfection practices for health care settings.
- Refer to the “Contact investigation” section to determine how to assess risk to exposed patients and provide disease control recommendations.
- Exposed patients without evidence of immunity to measles who did not receive PEP should be discharged as soon as possible and advised to continue to watch for measles symptoms for 21 days after discharge or last exposure date.
- Exposed patients without prior evidence of immunity to measles, regardless if they received PEP, who are unable to be discharged should be placed in airborne and contact precautions from Day 5 to Day 21 (Day 28 if IG PEP) after exposure.
- After the patient leaves the room, it should remain vacant for the appropriate time (up to two hours) to allow for 99.9% of airborne-contaminant removal. In the clinic, or when in doubt, vacate the room for two hours. Visit the appendix for Air guidelines from the Guidelines for Environmental Infection Control in Health-Care Facilities (2003).
Health care personnel exclusion
- Health care personnel need to meet one of these criteria as evidence of immunity:
- Documentation of two doses of live measles-containing vaccine, separated by at least 28 days, with the first dose on or after the first birthday.
- Documentation of a positive measles IgG test.
- Laboratory confirmation of a prior measles infection.
- Born before 1957.
- For unvaccinated HCP born before 1957 who lack laboratory evidence of measles immunity or laboratory confirmation of disease, health-care facilities should consider vaccinating HCP with 2 doses of MMR vaccine separated by 28 days.
- Health care personnel meeting the required evidence of immunity criteria may continue to work regular duties but should be instructed to watch for symptoms until 21 days after their last exposure and contact employee health if they develop symptoms. PEP is not necessary for these individuals.
- Health care personnel with one documented dose of MMR should receive an additional dose of MMR as soon as possible (at least 28 days after their first dose). Work restrictions are not necessary but the facility should implement daily monitoring for signs and symptoms of measles from the fifth day after their first exposure through the 21st day after their last exposure.
- Susceptible health care personnel who do not meet the above criteria and are exposed to measles should be relieved from patient contact and excluded from the facility from Day 5 after initial exposure to Day 21 after last exposure or until the facility is declared measles-free. PEP should be administered based on criteria above, but does not release a susceptible health care worker from exclusion after the exposure.
- Instruct health care personnel to immediately report any symptoms consistent with measles. Because of the nature of exposures in health care settings, testing of these staff should be prioritized at the CDPHE Lab. Healthcare personnel with symptoms suggestive of measles should be excluded from work until public health evaluation.
- Health care personnel who develop measles should be isolated at home and excluded from work until four days after rash onset.
- Health care personnel who test positive for measles and do not develop a rash should be isolated at home and excluded from work until nine days after the first symptom onset.
Child care and schools
Case investigation in a child care or school facility
- Determine the dates the case attended or worked in child care or school while infectious. Consider:
- What classrooms they use,
- What other areas of the facility they visited,
- Was there any mingling with other grade levels or classrooms,
- Extracurricular activities,
- Before and after school care, and
- If school transportation was used.
- Staff and/or public health personnel should review the measles vaccination records of all children and staff at the facility to determine who at the facility is susceptible to measles.
- These guidelines may also apply to children’s camp settings (either day camps or residential camps). As camp settings and situations can vary greatly, consult with the CDPHE VPD Unit to determine the appropriate exclusion, monitoring, and quarantine guidance.
Exclusion
- Measles cases should be excluded from child care or school and isolated at home for four days after rash onset (day of rash onset is counted as day 0).
- Contacts who receive IG PEP should be excluded from child care classrooms with infants <12 months for 28 days. See below for additional recommendations of exclusion.
- Excluded students and staff are not to attend in-person school or child care or extracurricular activities such as clubs or sports, or camps.
Monitoring
- Exposed students and staff should monitor for symptoms for 21 days (or 28 days if they received IG), regardless of immunization status. Students and staff should report development of symptoms to public health immediately to quickly identify cases and prevent further spread.
Quarantine
- Quarantine may be recommended by public health for individuals who do not have evidence of immunity and did not receive PEP within the recommended time frame after exposure to measles.
- Quarantine is different from school exclusion as it requires avoiding all public places including places of work, stores, public transportation, and social gatherings, in addition to all school-related activities.
- Quarantine may not always be required when exclusion is recommended.
Exclusion of child care and school contacts by immune status
(regardless of vaccine exemption documentation)
Students and children with zero documented doses of MMR
- Infants aged 0-5 months old:
- MMR is contraindicated. They should receive IG PEP within six days of initial exposure to measles to prevent or lessen the severity of measles disease.
- Infants who receive IG PEP should be excluded from the child care facility through 28 days after their last exposure.
- Infants who do not receive IG should be excluded through 21 days after their last exposure.
- Infants aged 6-11 months old:
- Should receive one documented dose of MMR within 72 hours after their initial exposure to measles and may return to school immediately. The child will need to be vaccinated again according to the routine schedule (i.e., two additional doses, the first between 12-15 months of age. All doses of MMR must be separated by at least 28 days.)
- If unable to receive MMR within 72 hours but within six days from initial exposure, recommend the child receive IG to prevent severe measles infection. Infants who receive IG should be excluded from child care for 28 days.
- If unable to receive MMR or IG PEP within the recommended timeframes, they should be excluded from child care for the duration of their incubation period (21 days).
- 12 months and older:
- Should receive one documented dose of MMR within 72 hours after their initial exposure to measles and may return to school immediately. A second dose of MMR will need to be received at least 28 days later to complete the two-dose series.
- If unable to receive MMR PEP within 72 hours after the initial exposure to measles, exclude from school seven days from initial exposure through 21 days after the last known case was present in the school/child care facility while infectious, or through 21 days after their last exposure to a case; whichever is later.
- Unvaccinated students should still be recommended to receive MMR vaccine to provide protection against future measles exposures. Students vaccinated after 72 hours may not need to be excluded from school if additional cases present.
- A student or child who remains unvaccinated may have their initial exclusion period extended beyond 21 days if they do not receive a dose of MMR and additional cases present, since the presence of additional cases might result in additional exposures.
- Students in this age group who qualify for IG should receive IG PEP within six days of initial exposure to measles. Exclusion from school for 28 days should be considered and is dependent on factors such as intensity and duration of their exposure, the vaccination coverage of the school or child care, and the presence of populations at risk for severe measles disease.
Students with one documented dose of MMR
- Infants aged 6-11 months old:
- Infants in this age group who received one early documented dose of MMR do not need to be excluded from child care. Once they are 12 months old, they will need to follow the recommended vaccination schedule for MMR.
- Child care and preschool children (up to 6 years):
- May continue with regular school activities and do not need to be excluded.
- An early second dose of MMR may be required to return to child care or preschool during an outbreak.
- School age students K-12:
- Students in this age group should receive their second dose of MMR as soon as possible. These students may be excluded from school during an outbreak until they receive a second dose of MMR. In these situations, students can return to school once they receive their second MMR.
- Schools with low vaccination rates might have additional requirements, such as exclusion until they receive their second MMR dose
Students with two documented doses of MMR
- Are likely to be immune to measles and can continue regular school activities.
Staff or adults working or volunteering within child care or school
- Adults with presumptive evidence of immunity do not need to be excluded.
- Public health may require staff closely working with infants to receive a second dose of MMR to not be excluded from work.
- During an outbreak, all adults may be required to receive a second dose of MMR to return to work within child care or school.
- Adults that also have a role in health care (e.g., school nurse) need to meet health care personnel criteria.
- Adults that do not have presumptive evidence of immunity prior to exposure and receive one documented dose of MMR within 72 hours of initial exposure to measles may return to work immediately.
- Adults without presumptive evidence of immunity that do not receive a dose of MMR within 72 hours of initial exposure to measles may be excluded from Day 7 of initial exposure through 21 days after the last known case was present in the child care or school while infectious, or through 21 days after their last exposure to a case; whichever is later.
- Unvaccinated staff unable to receive MMR within the 72-hour PEP window should still be recommended to be vaccinated to provide protection against future exposures.
- Adults who are unable to receive MMR after exposure to measles, but qualify for IG PEP, should receive IG PEP within six days of initial exposure to measles and public health could consider return to work with symptom monitoring for 28 days.
Notifications
- Recommend that the child care and school notify parents/guardians/caregivers, staff, and anyone entering the facility of the possible exposure to measles. CDPHE or the local public health agency can provide a sample letter for distribution.
- Child care and school personnel should immediately report all suspected measles cases to CDPHE or their local public health agency.
- Refer child care providers to the CDPHE guidelines, “Infectious disease guidelines in child care and school settings” for additional measles information.
Higher Education
Case Investigation
- Determine the dates the measles case attended school while infectious including what dorm they live in (or other congregate living situation like a fraternity/sorority house), classes they attended, what other areas or locations on campus they visited, extracurricular activities, events (sports), and if any public transportation was used.
- School and/or public health personnel should assess the immunity of students and staff directly exposed to a measles case in classrooms, dorm/congregate rooms, and other shared spaces by reviewing measles immunization records. If possible, colleges should provide a list of students and staff exempt from vaccination to public health.
Exclusion
- Measles cases should be excluded from school and isolate themselves at home during their infectious period (through four days after rash onset).
- If they are unable to go home, they should be alone in a dorm room or some other single occupancy room, keep the door closed, and arrangements should be made to drop off food and medicine.
- Excluded students and staff may not attend in-person school, extracurricular activities, or social events.
Exclusion of higher education setting contacts by immune status
(regardless of vaccine exemption documentation)
Students in higher education settings with zero documented doses of MMR:
- Should receive one documented dose of MMR within 72 hours after their initial exposure to measles and may return to school immediately. A second dose of MMR should be administered at least 28 days later to complete the two-dose series.
- If unable to receive a dose of MMR within 72 hours after the initial exposure to measles, exclude from school through 21 days after the last known case was present in the school while infectious, or through 21 days after their last exposure to a case; whichever is later.
- Unvaccinated students should still be recommended to receive MMR beyond 72 hours to protect against future measles exposures.
- Students vaccinated after 72 hours will not need to be excluded from school if additional cases present.
- In the event of an outbreak and widespread exposures public health may consider re-admitting unvaccinated students at the time of vaccination if allowing these students back at school increases overall vaccination coverage and school productivity.
- Unvaccinated students who are unable to receive MMR after exposure to measles, but qualify for IG PEP, should receive IG PEP within six days of initial exposure to measles and public health could consider return to school with symptom monitoring for 28 days.
Students in higher education settings with one documented dose of MMR
- Students should be recommended to receive their second doses of MMR as soon as possible and may be excluded from school and activities during an outbreak until they receive a second dose of MMR.
Students in higher education settings with two documented doses of MMR
- Are likely to be immune to measles and can continue regular school activities.
Staff or adults working or volunteering within the higher education facilities
- See Staff/Adults section under child care and schools section.
Monitoring
All exposed students and staff should monitor for symptoms for 21 days (or 28 days if they received IG PEP). Students and staff should report development of symptoms to public health immediately to quickly identify cases and prevent further spread.
Quarantine
- Quarantine may be recommended by public health for individuals who do not have prior evidence of immunity and who do not receive PEP within the recommended time frame after exposure to measles.
- Quarantine is different from school exclusion as it requires avoiding all public places including places of work, stores, public transportation, and social gatherings, in addition to all school-related activities.
- Quarantine may not always be required when exclusion is recommended.
Notifications
- The school should notify students, staff, and anyone entering the facility of the possible exposure to measles. CDPHE or the local public health agency can provide a sample letter for distribution.
- School personnel should report all suspected measles cases to CDPHE or their local public health agency.
Jails and detention centers
- People suspected of having measles should be immediately reported to the state or local public health department and isolated from other people who are incarcerated or detained, including not participating in work or other activities that put them in contact with potentially susceptible people until it is determined they don’t have measles through either lab testing or consultation with the state of local public health department.
- People confirmed to have measles should be isolated for the duration of their infectious period (four days prior to rash onset to four days after rash onset [day of rash onset is counted as day 0]).
- Staff suspected of having measles should not come to work.
- Determine dates the measles case was infectious and identify exposed people who are incarcerated or detained, staff, and visitors.
- Determine the measles immunity status of exposed personnel and people who are incarcerated or detained.
- IG PEP should be administered to exposed susceptible incarcerated or detained people and staff at increased risk of developing measles complications following recommendations in the Red Book, such as those who are severely immunocompromised or are pregnant.
Exclusion of contacts (staff and people who are incarcerated/detained) by immune status
Staff or people who are incarcerated or detained with no documentation of presumptive immunity
- If the exposed person without evidence of immunity receives one documented dose of MMR within 72 hours after their initial exposure to measles, they may return to normal activities and work immediately.
- If the exposed person without evidence of immunity does not receive a dose of MMR within 72 hours after the initial exposure to measles, they must be excluded from work and activities through 21 days after the last known case was present in the facility while infectious, or through 21 days after their last exposure to a case outside of the facility; whichever is later.
- If individuals are vaccinated outside of the 72-hour PEP window, they should remain excluded for only the duration of their incubation period. The vaccination after the 72-hour window would provide protection against new exposures.
- IG PEP should be administered to exposed susceptible incarcerated or detained people and staff up to six days after exposure if at increased risk of developing measles complications following recommendations in the Red Book.
Staff or people who are incarcerated or detained with documentation of presumptive immunity
- Individuals with at least one documented dose of MMR on or after their first birthday, do not need to be excluded.
- Staff that work in health care will need documentation of a positive measles IgG test OR documentation of two doses of measles-containing vaccine given in 1968 or later, separated by at least 28 days, with the first dose on or after the first birthday.
- Individuals born before 1957 are presumed immune to measles and do not need to be excluded.
- Individuals that provide laboratory evidence of immunity (positive measles IgG result) do not need to be excluded.
Monitoring
All exposed individuals need to monitor for symptoms for 21 days (28 days if they received IG), regardless of immunization status. Staff should report development of symptoms to public health immediately to quickly identify cases and prevent further spread.
Quarantine
Quarantine may be recommended by public health for those individuals that do not have any prior evidence of immunity who do not receive PEP within the recommended time frame after exposure to measles.
Airlines
- Measles cases should not travel by airplane until four days after rash onset (day of rash onset is counted as day 0).
- For measles cases who report airline travel while infectious, obtain detailed flight information including flight numbers, airline, date and time of travel, seat number, and who the case sat next to (i.e., their family member, a friend, or a stranger).
- CDPHE will notify the CDC Quarantine Station to investigate and follow up on measles cases on domestic and international flights. Notify a CDPHE VPD epidemiologist if a measles case was on a flight while infectious.
Specimen collection instructions, questionnaires for suspect cases, tools to help determine susceptibility to measles, and other resources to use during an investigation are available on CDPHE’s measles webpage.
CDC’s guidelines for measles PCR, virus isolation, and serology.
American Academy of Pediatrics (Red Book). Measles. Red Book 2024-2027: Report of the Committee on Infectious Diseases, 33rd Edition. Illinois, American Academy of Pediatrics, 2024.
Centers for Disease Control and Prevention. Epidemiology and Prevention of Vaccine-Preventable Diseases. Hamborsky J, Kroger A., Atkinson W, Wolfe S, eds. 14th ed. Washington DC: Public Health Foundation, 2021 or https://www.cdc.gov/vaccines/pubs/pinkbook/index.html.
Centers for Disease Control and Prevention. Manual for the surveillance of vaccine-preventable diseases. Centers for Disease Control and Prevention, Atlanta, GA, 2019.
Centers for Disease Control and Prevention. Measles- United States, January 1, 2020 - March 28,2024. MMWR, April 11, 2024; 73(14); 295-300
Centers for Disease Control and Prevention. National Notifiable Diseases Surveillance System. 2013 Measles Case Definition. January 2013. Accessed on-line January 2013.
Centers for Disease Control and Prevention. Prevention of Measles, Rubella, Congenital Rubella Syndrome, and Mumps, 2013: Summary Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR, June 14, 2013; 62(RR04);1-34