Introduction: infectious diseases in child care and school settings
On this page
Infectious disease in child care and school settings
Infectious diseases are caused by organisms such as bacteria, viruses, and parasites. Some infectious diseases can be spread from one person to another. Illnesses caused by infectious diseases are a common occurrence in children in child care and school settings. Child care providers, child care health consultants, school personnel, and school nurses should be aware of infectious diseases that affect children and be familiar with how to minimize their spread. These guidelines address infectious diseases often seen in children and provide ways to prevent, reduce, and control their spread. Most cases of illness are isolated to one child, but occasionally, an outbreak of a particular disease can occur in a child care or school setting. Unless otherwise specified, an outbreak means an increase in disease symptoms or illness regardless of a clinical diagnosis or laboratory testing in staff/children at more than expected levels. As few as two individuals (children or staff) in the same group with similar symptoms may constitute an outbreak. Outbreak reporting should not be delayed due to lack of diagnostic testing. Suspected outbreaks of any disease in any setting must be reported to the state or local public health agency immediately.
These guidelines are based on current health information. Recommendations for handling infectious disease issues in child care and school settings may change as new information becomes available. In addition, new infectious disease concerns sometimes emerge. The Communicable Disease branch at the CDPHE can help child care providers, child care health consultants, school personnel, and school nurses when infectious disease issues arise and can be reached at 303-692-2700. Local public health agencies are also available for consultation on infectious disease issues. Find your local public health agency and its contact information.
Public health reporting requirements, case investigation, and outbreak investigation
By law, certain diseases and conditions are reportable to public health for surveillance and investigation purposes and to implement disease control measures. Per Colorado regulation 6 CCR 1009-1 “Rules and Regulations Pertaining to Epidemic and Communicable Disease Control,” people either treating or having knowledge of a reportable disease, whether the disease is suspected or confirmed, must report the case to the state or local public health agency. This includes schools and licensed child care providers. A list of diseases and conditions reportable in Colorado is available on the Reportable Communicable Diseases and Condition table, as well as on CDPHE’s Report a Disease page. This website also contains a link to the Colorado statutes and regulations that address disease reporting.
When a suspected or confirmed disease case is reported, public health agencies may conduct an investigation to confirm the diagnosis, assess treatment options (if applicable), determine the cause of the illness, determine if anyone else has been exposed, and implement appropriate methods of disease control. Outbreaks of any disease, in any setting, must be reported to the state or local public health agency immediately. In an outbreak situation, the state or local public health agency will work with the child care facility or school to achieve the following.
Outbreaks of any disease, in any setting, must be reported to the state or local public health agency immediately. In an outbreak situation, the state or local public health agency will work with the child care facility or school to achieve the following:
- Control and prevent further spread of disease;
- Identify ill people so they can receive proper treatment if indicated;
- Attempt to identify the source of the outbreak;
- Determine who might have been exposed to the source or ill people;
- Identify infection risk factors;
- Evaluate existing prevention strategies.
Child care facilities and schools can also contact the state and/or local public health agencies about infectious conditions that are not reportable, especially if the facility has questions about notifying parents, exclusion, and disease control measures. School and facility closure recommendations are made on a case-by-case basis and consider factors such as attendance of students/children and staff, disease or illness severity, and vulnerability of children and staff. Consultation with local or state public health staff can help inform a facility administration’s decision to close due to illness.
Per the “Rules and Regulations Governing the Health and Sanitation of Child Care Facilities in the State of Colorado”, in addition to consulting with the state or local public health agency, child care facilities should also consult with their child care health consultant about any type of communicable disease issue, case, or outbreak. Child care facilities are inspected routinely by either the state or local public health agency to ensure compliance with the health and sanitation regulations. These inspections are typically conducted by Environmental Health Specialists employed at the state/local public health agency. It is acceptable for a child care facility to report cases of illness or outbreaks to the Environmental Health Specialist who conducts the health and sanitation inspections. Typically, the Environmental Health Specialist will then consult with the public health nurse or epidemiologist within his/her public health agency or at CDPHE to determine the best course of action.
To report a suspected or confirmed disease case or outbreak, please contact your local public health agency (contact information can be found at the link) or CDPHE at 303-692-2700 or 800-866-2759 (after-hours: 303-370-9395). To the extent it is available, the following information should be reported for all suspected or confirmed cases:
- Diagnosis.
- Patient’s name.
- Date of birth.
Sex. - Race and ethnicity.
- Address (including city and county).
- Phone number.
- Parent/Guardian name.
- Preferred language.
- Name and address of the responsible health care provider.
- Laboratory test results.
- Case suspected or confirmed.
Schools, public health reporting, and FERPA
Regarding student confidentiality and privacy, the federal Family Educational Rights and Privacy Act (FERPA) prohibits sharing of health-related information except in certain well-defined circumstances, including but not limited to: specified officials for audit or evaluation purposes, and appropriate officials in cases of health and safety emergencies. Notifying the state or local public health agency of a reportable disease in a student or an outbreak in a school does not breach FERPA confidentiality laws. In these situations, schools may disclose personally identifiable information to public health officials without prior parent consent. Additional information can be found on the U.S. Department of Education’s Family Educational Rights and Privacy Act (FERPA) webpage.
Informing parents/guardians of illness in the facility
When a child care facility or school has a child or staff member ill with an infectious disease, the question often comes up as to whether the facility needs to send a letter home to parents/guardians/caregivers of other children, or post a notice at the facility informing parents/guardians/caregivers of the illness. This is often dependent on the disease, the potential risk of spread to others, the presence of symptoms in other children/staff, and policies in place at the facility. Public health can help a facility or school in determining whether or not a letter or notice is necessary. In outbreak situations, it is common for public health to work with the facility or school to draft a letter to share with parents/guardians/caregivers, as well as a health alert to distribute to health care providers in the area. Additional information about sharing information is included at the U.S. Department of Education’s Family Educational Rights and Privacy Act (FERPA) webpage.
Exclusion guidelines for children and staff
Excluding children
Excluding a child who has an infectious disease from attending child care or school may decrease the spread of illness to others. The decision to exclude is typically based on the disease, and it should be made in conjunction with the school nurse or the child care health consultant, state or local public health agency, health care professionals, and parents/guardians. Exclusion recommendations are included for each disease or condition addressed in these guidelines.
In situations in which a child does not have a diagnosed disease/condition but has signs or symptoms indicative of a potentially infectious disease, exclusion may also be warranted. Generally, if any of the following conditions apply, exclusion from child care or school should be considered:
- The child does not feel well enough to participate comfortably in usual activities.
- The child requires more care than the child care or school personnel are able to provide.
- The child is ill with a potentially contagious illness, and exclusion is recommended by a health care provider, the state or local public health agency, or these guidelines.
- The child has signs or symptoms of a possible severe illness, such as trouble breathing.
- The facility is experiencing an outbreak.
In cases in which unprotected (unvaccinated/non-immune) children are exposed to a vaccine preventable disease (such as measles, mumps, rubella, and pertussis), the state or local public health agency should be consulted in order to determine if exclusion of unprotected children is necessary.
The chart below lists common symptoms that could possibly be related to an infectious disease. The chart indicates whether it is recommended to exclude a child exhibiting a particular symptom from child care or school. If a child is excluded based on symptoms (and not a diagnosed illness), the child should be allowed to return to child care or school once symptoms have subsided, or a health care provider clears the child or determines the illness is not communicable, provided that the child can participate in routine activities. CDPHE has another tool called “How Sick is Too Sick” that can help school and child care staff, and parents/guardians/caregivers determine if a child should stay home due to illness.
When a child has symptoms while at the school or child care facility, the following actions should be taken:
- Inform the school nurse, child care health consultant, or designated staff of the symptoms.
- Separate the ill child from the other children.
- Document the symptoms on the illness log.
- Sample illness log
- Take the child's temperature and record it on the illness log.
- If a child is coughing or sneezing, remind them to cover their mouth and to wash their hands afterward.
- After you touch an ill child, avoid touching other children until you have washed your hands.
- Inform the ill child’s parents/guardians of the symptoms. If it is determined that the child needs to be excluded, keep the ill child separated from other children until the parent/guardian/caregiver can pick up the child.
- Equipment, bedding, or toys used by the ill child should be cleaned and sanitized or disinfected afterward.
Excluding staff
Occasionally, child care and school personnel become ill with an infectious disease. When this occurs, the child care facility or school should consult with the state or local public health agency to determine whether the ill staff member can work. If ill with diarrhea or vomiting, child care and school personnel should not work until at least 24 hours after the last episode of vomiting or diarrhea. This is especially important for staff that work in food service or handle food in any manner and for staff that work with infants and toddlers (including staff that prepare and serve bottles to infants/toddlers). During an outbreak or diagnosis with some infectious pathogens, staff may be required to be excluded for longer than 24 hours. Consult state or local public health if a staff member has an infectious disease diagnosis.
Considerations for children who are developmentally disabled or immunocompromised
Disease control guidelines for children with developmental disabilities or who are immunocompromised may be different than the guidelines presented in this document. In situations where a child with developmental disability or who is immunocompromised has an infectious disease or is exposed to another child with an infectious disease, the child care health consultant or school nurse should be consulted. The state or the local public health agency is also available for consultation.
Illness transmission
Infectious diseases can be spread in a variety of ways, referred to as transmission routes.
Droplet transmission / Infectious discharges
Diseases with respiratory tract symptoms (runny nose, cough, sore throat, sneezing) are often spread by droplets containing viruses or bacteria or by surfaces contaminated with nose/throat discharges from people with infection. Droplets are generated during coughing, sneezing, or talking. These “large” droplets generally travel less than three feet before falling to the ground and do not remain suspended in the air. Before falling to the ground, droplets may be deposited on the mucous membranes of the eye, nose, or mouth of another person within three feet, resulting in disease transmission. In addition, sick people, especially children, will often contaminate their hands and other objects with infectious nose/throat discharges. When another person comes in contact with these objects and then touches their eyes, mouth, or nose, they can become infected. This type of transmission route is common in child care and school settings. Some of the infections passed in this way are the common cold, SARS-CoV-2, chickenpox, croup, fifth disease, hand, foot and mouth disease, influenza, meningitis (viral and bacterial), mumps, rubella, pertussis (whooping cough), pink eye (conjunctivitis), RSV, and strep throat.
Airborne transmission
This mode of transmission is rare and only a few diseases are spread by this route (such as SARS-CoV-2 in some circumstances and conditions, measles, and tuberculosis). Airborne transmission occurs when a person with infection coughs, sneezes, or talks and generates very small respiratory particles (droplet nuclei) containing viruses or bacteria. These small particles remain suspended in the air for long periods and can be widely dispersed by air currents. When another person inhales these small particles, they can potentially become ill.
Fecal → oral transmission
Intestinal tract infections are often spread through oral ingestion of viruses, bacteria, or parasites found in the stool of a person or animal with infection. This type of transmission happens when objects contaminated with microscopic amounts of human or animal feces are placed in the mouth. In child care and school settings, the most frequently contaminated objects and areas are hands, diaper changing tables, classroom floors, faucet handles, toilet flush handles, toys, and tabletops. However, almost anything may become contaminated with feces. Fecal→oral transmission can also occur when food or water is contaminated with microscopic amounts of human or animal feces and then ingested. Organisms spread by this transmission route include: Campylobacter, Clostridioides difficile, Cryptosporidium, Shiga toxin-producing E. coli (which includes E. coli O157:H7), Giardia, hepatitis A, Salmonella, Shigella, and a variety of intestinal viruses like norovirus. Other infections like hand, foot, and mouth disease, and viral meningitis can also be spread through this route.
Skin contact/direct contact
Some infections can be spread directly by skin-to-skin contact, or indirectly by contact with contaminated surfaces like clothing. Chickenpox (varicella), shingles (herpes zoster), herpes, head lice, impetigo, molluscum contagiosum, MRSA, ringworm, scabies, and tetanus are all spread this way.
Blood/body secretions contact
Some infections are transmitted when a cut or mucous membrane (linings of various body parts and internal organs) comes in contact with the blood or other body secretions like saliva, urine, and seminal and cervical fluids of a person with infection. This type of transmission is very rare in child care and school settings. Diseases such as hepatitis B, hepatitis C, and human immunodeficiency virus (HIV) can be spread by contact with infected blood. Infected children can possibly transmit these infections through biting if there is visible blood mixed with their saliva (i.e., from bleeding gums). CMV (cytomegalovirus) can be spread by body secretions like urine and saliva, and mononucleosis and some forms of bacterial meningitis can be spread by saliva.
Sexually-transmitted infections (STI)
These infections are most commonly transmitted by sexual contact, including genital-to-genital, oral-to-genital, or genital-to-anal contact. HIV and AIDS, chlamydia, genital herpes, genital warts, gonorrhea, hepatitis B, pubic lice (crabs), and syphilis can be spread in this way. The possibility of sexual abuse must be considered when infections occur in prepubescent children and must be reported to appropriate authorities. The Colorado Child Abuse and Neglect Hotline for reporting possible abuse or neglect is 844-CO-4-KIDS (844-264-5437).
Appropriate antibiotic use
- Antibiotics are important drugs that treat infections caused by bacteria. Antibiotics save lives, but they can also be harmful if prescribed when not needed. Harms include side effects and the development of antibiotic resistant bacteria. Prescribers should seek to prescribe antibiotics only when indicated, choose the most appropriate antibiotic for the suspected infection, and use the shortest effective duration of antibiotic therapy. Unfortunately, approximately half of outpatient antibiotic prescriptions are inappropriate, and up to one-third are unnecessary. Here are some tips for appropriate antibiotic use:
- Antibiotics do NOT treat viruses, like those that cause colds, flu, respiratory syncytial virus (RSV) or COVID-19. Antibiotics do not treat a runny nose, even if the mucus is thick, yellow, or green.
- Antibiotics are only needed for treating certain infections caused by bacteria, but even some bacterial infections get better without antibiotics. Antibiotics aren’t needed for many sinus infections, most bronchitis infections, and some ear infections.
- An antibiotic will not make a person feel better if they have a virus. Respiratory viruses usually go away in a week or two without antibiotics. Parents/guardians should be advised to talk with their child’s health care provider about the best way to feel better while their body fights off the virus.
- Taking antibiotics can create resistant bacteria. Antibiotic resistance occurs when bacteria develop the ability to defeat the drugs designed to kill them. If antibiotics lose their effectiveness, we lose the ability to treat infections.
- If a person needs antibiotics, they need to take them exactly as prescribed.
- Parents/guardians should talk with their child’s doctor if the child develops any side effects, especially diarrhea, since that could be a C. difficile (C. diff) infection which needs to be treated right away.
- Antibiotics aren’t always the answer. Everyone can help improve antibiotic prescribing and use.
CDC has handouts, posters, prescription pads, recommendations for symptom relief, communication strategies, and other educational resources for parents/guardians and health care providers: Antibiotic Use | CDC.
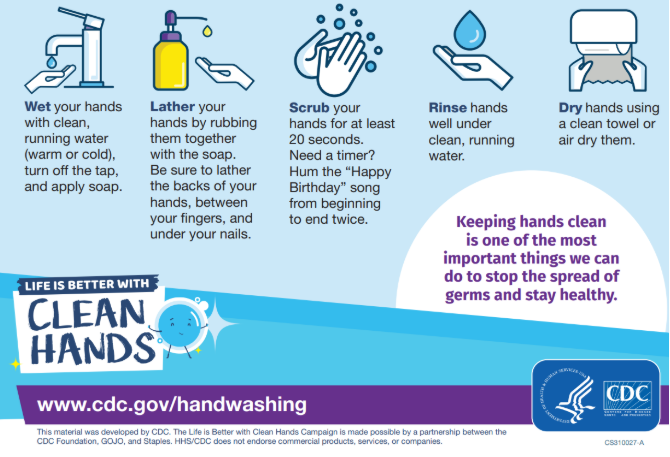
Disease prevention: Hand hygiene
Hand hygiene is one of the best tools for controlling the spread of infections. All children and staff should perform effective hand hygiene, which will reduce the amount of illness in child care and school settings.
- Hand hygiene with soap and water:
- Use SOAP and WARM RUNNING WATER.
- Rub hands vigorously as you wash them.
- Wash ALL surfaces including the backs of hands, wrists, in-between fingers, and under fingernails.
- Wash for at least 20 seconds. (if you don’t have a timer, hum the “Happy Birthday” song from beginning to end twice).
- Rinse hands well.
- Dry hands with a clean paper towel or air dryer.
- If using paper towels, turn off the water using a paper towel instead of bare hands.
- If cloth towels are used, they must be laundered after each use.
State health regulations for schools require that soap and paper towels or air dryers be available for all bathroom facilities. Schools often have a problem keeping the restrooms stocked with soap and paper towels due to children playing with the items and clogging toilets or making messes. Schools must find solutions to these problems rather than removing soap and paper towels from the restrooms.
When to wash hands:
- When arriving in the classroom at the beginning of each day.
- Before, during, and after preparing or serving food to children.
- Before eating (children in child care settings must also wash their hands after eating).
- Before and after caring for someone who is sick.
- Before and after administering medication.
- Before and after caring for a cut or wound.
- Before and after handling or playing on a sensory table.
- After returning to the classroom fro outside time.
- After coughing, sneezing, and/or wiping your nose or someone else’s nose.
- After using the toilet.
- After changing diapers (wash both the staff’s and child’s hands).
- Before and after administering first aid.
- After cleaning.
- After touching an animal, animal feed, or animal waste.
- After handling pet food or treats, or touching an animal’s cage or enclosure.
- After handling garbage.
- Whenever hands are visibly dirty.
- Children who are unable to wash their hands should have assistance from staff.
- Food handlers are required to wash hands before preparing and handling food and when hands are soiled.
Hand hygiene with soap and water:
Hand sanitizer
Alcohol-based hand gels can quickly reduce the amount of germs on hands in some situations. Hand gels do not eliminate all types of germs and are not as effective when hands are visibly dirty or greasy. Children should be supervised when using these products and they should only be used on children aged 3 and older. The rules and regulations governing both schools and child care prohibit the use of hand sanitizer in lieu of handwashing. It is recommended that these products be used in addition to regular handwashing and only used as the main method of handwashing when facilities are not readily available, such as on a field trip.
Disease prevention: Immunizations
Childhood immunizations
Immunizations help prevent serious illnesses. Originating in the 19th century, state-based school immunization laws are a key public health strategy. This “system of immunization” or “system of prevention” works year-round to support high vaccination coverage and low rates of vaccine-preventable diseases (VPDs).
Colorado law requires children attending Colorado licensed child cares and schools to be up to date or in the process of getting up to date for all school-required vaccines, unless an exemption is on file at the school.
Refer to the immunization requirements for school entry webpage for more information.
The vast majority of families vaccinate their children. When making the decision to vaccinate, families can be confident that their choice is supported by science and the nation’s leading medical and health organizations, including:
- American Academy of Pediatrics (AAP)
- American Academy of Family Physicians (AAFP)
- American Medical Association (AMA)
- American Nurses Association (ANA)
- Many other organizations and professional societies
These leading experts study and understand the benefits and risks of vaccines and strongly recommend vaccination as the best way to protect children, families, and communities against serious preventable diseases.
Refer to the appropriate webpage for immunization requirements to attend child care or preschool, school (K-12), camp, or college or university.
Adult immunizations
Vaccines help adults stay healthy too!. It is strongly recommended that child care and school personnel be vaccinated (or have proof of immunity) against many of the diseases that vaccines can prevent. Staff who work in child care and school settings should reference Immunize.org’s Vaccine for Adults (PDF) resource as a quick guide for adult vaccine recommendations.
Child care and school personnel who are exposed to a vaccine-preventable illness, or who work in a setting experiencing an outbreak of vaccine-preventable illness, may be excluded from work if they lack proof of immunity (e.g., documented vaccination or an antibody titer indicating immunity).
Disease prevention: Covering coughs
Influenza and other respiratory illnesses can be spread by coughing, sneezing, or unclean hands. To help prevent the spread of these illnesses, children and staff should try to use proper cough etiquette, including:
- Cover your mouth and nose with a tissue when you cough or sneeze.
- Put used tissues into the trash.
- If a tissue is not available, cough or sneeze into your upper sleeve or elbow, instead of the hands.
- Wash your hands often using proper technique.
Educational materials on cough etiquette for school and child care settings can be found on CDC’s Influenza webpage.
Disease prevention: Food safety
Foodborne illness can often be prevented by adhering to the following safe food handling guidelines:
- Train all food handling staff on food safety.
- Children and staff handling food must wash their hands prior to handling food. A sink dedicated to handwashing must be used; sinks intended for food preparation must not be used for handwashing unless approved by CDPHE or the local health department.
- Ready-to-eat foods such as salads, sandwiches, fruit, and any food that is not going to be cooked prior to consumption, must not be prepared or handled with bare hands. Gloves are required when handling ready-to-eat foods.
- Wash hands and change gloves between working with raw meats/poultry and ready-to-eat foods.
- Ill children and staff must not handle food, especially if they are ill with gastrointestinal symptoms, such as vomiting or diarrhea.
- Children or staff with skin lesions on exposed areas like the face, hands, and fingers must not handle food unless the wound is covered with a waterproof bandage and gloves are worn for all food handling activities.
- Store food at proper temperatures. Potentially hazardous cold foods like eggs, milk, dairy products, meat products, etc. must be stored at 41°F or below. Hot foods must be held at 135°F or above.
- Meat and poultry products must be cooked to the proper temperature. Ground beef must be cooked to an internal temperature of 155°F.
- Poultry must be cooked to 165°F. A complete list of cook temperatures and other food safety resources can be found here.
- The facility must have a calibrated thermometer to check food temperatures.
- Thaw food in an appropriate manner, such as in the refrigerator, under continuously running cold water in a continuously draining sink, or in the microwave immediately before serving or cooking.
- Raw meat and poultry must be stored on the bottom shelf of the refrigerator to prevent contamination of other food items.
- Thoroughly wash fresh produce in a clean and sanitized food preparation sink before preparation. This includes fruits with a peel, such as cantaloupe, watermelon, and avocado prior to cutting.
- Use an approved food contact surface sanitizer on all food contact surfaces. Have appropriate test strips on hand to check the sanitizer concentration to ensure it is at proper levels, unless it is manufactured as a ready-to-use product.
- Avoid cross-contamination by washing and sanitizing hands, cutting boards, utensils, and dishes between different foods. Sanitize cutting boards, utensils, and dishes with an EPA-approved sanitizer.
- Use separate cutting boards for produce and raw meats/poultry.
- All food products must be stored away from medications, first aid supplies, cleaning products, and other chemicals.
- Do NOT serve unpasteurized products such as milk, cheese, other dairy products, or juice in the facility or during field trips.
- For regulations covering infant feeding (hygienic practices, food storage, handling bottles, and solid food), please reference Section 7.12 in the Colorado “Rules and Regulations Governing the Health and Sanitation of Child Care Facilities in the State of Colorado.”
For additional information on food safety, please consult with the state or local public health agency.
Disease prevention: Facility environment
Keep age groups separate
Separating children by age groups, particularly in child care facilities, helps to prevent the spread of infections to other groups of children and staff; ill children who are being sent home should also be separated from other children until they are picked up.
Meal times
Only authorized food handlers should enter kitchen areas to avoid contamination and transmission of disease. Children should not share food, plates, or utensils. Tabletops should be cleaned and sanitized before meals and between different groups of children using the tables. For child care facilities, use a separate utensil for each baby. For meals served family style, clean utensils should be provided for each dish. Children should be supervised while serving themselves to assure they are using utensils to prevent contamination of food. If food does become contaminated, it must be discarded. Each family style serving dish should be clean and sanitized before it is filled or refilled. This means serving dishes returned to the kitchen for seconds should be washed and sanitized, and a new serving should be served on clean, new plates. During an outbreak of communicable disease, facilities may be required to cease family style meal service.
Nap times (for child care facilities)
Children should be provided with their own crib (for infants), cot or mat (for older children). If this is not possible, they should be provided with their own set of mattress covers and linens, which should be laundered weekly either at the facility or sent home with the family. Mattresses, mats, and cots must be cleaned and sanitized between use by different children.
Cleaning, sanitizing, and disinfecting
Cleaning, sanitizing, and disinfecting surfaces in school and child care settings will help prevent transmission of infectious diseases. These terms all have different meanings and involve different types and concentrations of chemicals/solutions.
- Cleaning removes visible soil and debris and is done before sanitizing or disinfecting. Cleaning solutions are typically detergent and water.
- Sanitizing kills 99.9% of microorganisms on a surface, so it is unlikely that people having contact with a sanitized surface would be exposed to disease-causing organisms. Unscented household chlorine bleach mixed with water is a common sanitizing solution, although other chemicals are available. Generally, a bleach solution made at a concentration of 50 to 200 parts per million is sufficient for routinely sanitizing surfaces that are not visibly soiled and is not toxic to humans. Because several different bleach concentrations are available for purchase, follow the mixing instructions for sanitizing on the specific bottle of bleach used. The solution must be tested when it is made to assure proper concentration. The solution must be tested daily if it is not discarded at the end of the day. If a school or child care center is using a sanitizer other than a bleach solution, staff should check with their local public health agency to ensure the chemical meets regulatory requirements. All sanitizing solutions should be stored in a labeled container out of the reach of children. The label must indicate what it is and how it is intended to be used (e.g., bleach water for tables and toys).
In classrooms with young children, toys must be washed, rinsed, and sanitized regularly. Toys that are soiled or placed in a child’s mouth must be washed, rinsed, and sanitized prior to use by another child. Toys used with infants and toddlers must be washed, rinsed, and sanitized daily. Toys used with preschool and older children must be washed, rinsed, and sanitized weekly or more often, if needed. Common areas, desks/tables, doorknobs and handles, faucet handles, toilet seats, and drinking fountains are examples of areas that should be kept clean and periodically sanitized. - A disinfectant may be used on common touch surfaces in schools, children’s resident camps, and other 24-hour child care facilities at the discretion of the program personnel provided labeled instructions are followed.
- Disinfecting kills nearly 100% of microorganisms on a surface, so it is very unlikely that people having contact with a disinfected surface would be exposed to disease-causing organisms. Unscented household chlorine bleach mixed with water (at higher concentrations than used for sanitizing solutions) is also commonly used as a disinfectant, although other chemicals are available. Use disinfectants according to the label on the product or EPA registration. A list of disinfectants that meet the approval criteria for child care facilities can be found on our child care health regulations webpage. In an outbreak situation, public health may recommend using an even stronger bleach solution for disinfecting surfaces, depending on the organism causing the outbreak. If a school or child care center is using a disinfectant other than a bleach solution or one that is on the disinfectant list, staff should check with their local public health agency to ensure the chemical meets regulatory requirements and is effective against norovirus. If a surface is contaminated with a bodily fluid or excretion like blood, vomit, or feces (such as on a diaper changing table), a disinfectant must be used following cleaning to ensure disease-causing organisms are destroyed. Toys or items that can be placed in a child’s mouth should be washed, rinsed, and sanitized after disinfection.
Soft furnishings and linens can be sanitized or disinfected through the use of a washing machine and dryer. This can be achieved by washing items in 140°F water, adding bleach or another laundry disinfectant in the rinse cycle, or by drying at a temperature of 140°F or greater.
Cleaning, sanitizing, and disinfection recommendations
Soft furnishings and linens can be sanitized through the use of a washing machine and dryer. This can be achieved by washing and drying items using the highest heat settings. Bleach or another laundry sanitizer should be added during the rinse cycle if items being laundered have been contaminated with high hazard body fluids, which include urine, feces, vomitus, blood, and other body fluids with blood present.
Diaper changing
Infections that are transmitted by the fecal→oral route can be spread by poor diaper changing procedures. To avoid this, always use the following method for changing diapers (note: the black text in the images below is required by the regulations; the orange text offers additional steps that can be taken):
CDPHE DEHS Diapering Procedure poster (April 2025) in English | Spanish
Toilet-training children
Soiled clothes must be placed in a plastic bag for parents/guardians/caregivers to take home at the end of the day. Parents should supply a clean change of clothes to the facility ahead of time in case of accidents. After helping children use the toilet, show them how to wash their hands. The use of potty chairs in child care facilities is not permitted.
Animals/pets at child care and school settings
Animals in the classroom can be beneficial in the education process. However, some animals can present potential health and safety risks to humans, including infectious disease transmission, bites, and allergies. For example, many animals, especially reptiles and live poultry like chicks and ducklings, shed Salmonella bacteria in their feces without being sick themselves. People can contaminate their hands with feces when they handle the animal, feed the animal, or clean up after the animal (such as cleaning the cage or other enclosure), and disease can spread through the fecal→oral route. Some animals are not appropriate for the classroom, such as: poisonous animals (like poisonous/venomous spiders, snakes, and insects); wild, stray, or aggressive animals; or animals from an unknown source. To minimize the risk of children and staff acquiring an infectious disease from an animal or from being bitten, simple precautions should be taken, as outlined below:
General information:
- Children (especially those aged 5 years and younger) must be supervised carefully when around animals and animal enclosures, especially if children are handling animals.
- Reptiles, amphibians, and live poultry (e.g., chicks and ducklings) are prohibited in classrooms and facilities with children who are kindergarten age or younger (younger than 5 years). This includes hatching eggs in an incubator.
- Inform parents/guardians of animals that are kept onsite or may be visiting the facility.
- Animal cages or enclosures must be kept clean and in good repair. Do not clean animal cages or enclosures in sinks or other areas used to prepare food and drink or used for handwashing. Children aged 5 years and younger must not clean enclosures.
- Children and staff must always wash their hands with soap and running water after any contact with animals, their cages or enclosures, or their food, and after visiting places with animals, such as zoos or farms.
- Children must never “kiss” animals or have them in contact with their faces.
- Do not allow animals to roam free in the facility.
- Do not allow animals in areas where food and drinks are prepared or consumed.
- Clean and disinfect all areas where animals have been present.
- Animals kept onsite must receive regular veterinary care and must be up to date on all recommended animal vaccinations.
School settings (K-12):
- If children older than 5 years of age assist in cleaning the cage or enclosure, they must be supervised and must wash their hands with soap and running water afterwards.
- Live poultry (e.g., chicks and ducklings), reptiles, and amphibians are prohibited from classrooms with children kindergarten age or younger or communal areas that these children use. Because infections from these animals spread via fecal→oral transmission (hand-to-mouth behaviors), having these animals in other classrooms where children engage in frequent hand-to-mouth behaviors is discouraged.
Child care and preschool settings:
- Live poultry (e.g., chicks and ducklings), reptiles and amphibians are prohibited in child care and school settings where children are kindergarten age and younger (younger than 5 years of age). This includes hatching eggs from an incubator.
- In facilities that also have kids kindergarten age and older (older than age 5), live poultry (e.g., chicks and ducklings), reptiles, and amphibians are prohibited from classrooms with children kindergarten age or younger or communal areas that these children use. This includes hatching eggs from an incubator. Because infections from these animals spread via fecal→oral transmission (hand-to-mouth behaviors), having these animals in other classrooms where children engage in frequent hand-to-mouth behaviors is discouraged.
- The following animals are also prohibited in all child care facilities: psittacine birds, ferrets, primates, poisonous fish, poisonous reptiles, poisonous amphibians, aggressive animals and fish, wild-caught animals, or any other animals which may pose a hazard to the health of the children.
- Children in child care settings can not assist in cleaning cages or enclosures.
- Exposure to farm animals such as goats, sheep, or cows is strongly discouraged in child care settings where children aged 5 years and younger are present due to the potential risk for disease transmission.
- Mobile petting zoos and other events where the public can interact with live animals are strongly discouraged from visiting child care settings where children aged 5 years and younger are present due to the potential risk for disease transmission. There is an exception for programs that are AZA accredited. More information can be found here.
“Compendium of Measures to Prevent Disease Associated with Animals in Public Settings” from the National Association of State Public Health Veterinarians provides recommendations for controlling disease and minimizing health risks associated with animal contact in a variety of settings. CDC also has information about the health risks of a variety of animals.
Resources
The following resources may be helpful when dealing with infectious disease issues in school and child care settings:
- American Academy of Pediatrics (AAP)
- Bloodborne Pathogens: Contact CDPHE at 303-692-2700
- Children’s Hospital Colorado - Denver (School Health Program: 303-281-2790)
- Colorado Department of Education (CDE) (School Nursing and Health Consultant: 303-866-6779)
- Colorado Department of Early Childhood (CDEC) Child Care Licensing: Main Phone: 800-799-5876)
- CDPHE (Main Phone: 303-692-2000 or 800-866-7689)
- CDPHE Child and Adolescent Health
- CDPHE Communicable Disease Branch (Main Phone: 303-692-2700 or after hours 303-370-9395 for urgent situations)
- CDPHE Hepatitis Program (Main Phone: 303-692-2700)
- CDPHE Immunization Program (Main Phone: 303-692-2700)
- CDPHE Sexually Transmitted Infections Office (Main Phone: 303-692-2700)
- CDPHE Tuberculosis Program (Main Phone: 303-692-2700 or TB Program Direct Line: 303-692-2750)
- Healthy Child Care Colorado (Main Phone: 303-339-6800)
- Local public health departments and/or environmental health services
- Rocky Mountain Poison and Drug Safety Center (Main Phone: 800-222-1222)
Publications
- “The Red Book,” published by the American Academy of Pediatrics
- “Control of Communicable Diseases Manual,” published by the American Public Health Association
- “Managing Infectious Diseases in Child Care and Schools,” (The Purple Book), published by the American Academy of Pediatrics
- “Family Educational Rights and Privacy Act (FERPA)” U.S. Department of Education